
12/08/2025 - Press release
Adding a MET gene inhibitor enhances the effect of combined chemotherapy and immunotherapy in small cell lung cancer (SCLC), according to a multicenter study led by the Hospital del Mar Research Institute, in collaboration with researchers from the CIBERONC cancer research network. The study, published in Cell Reports Medicine, highlights the role of HGF (hepatocyte growth factor)-which is linked to cell proliferation and survival-in the poor prognosis of this disease and its resistance to treatment. The research explores a novel approach that adds a MET inhibitor to standard therapy and demonstrates improved treatment response.
Small cell lung cancer is one of the most aggressive types of lung cancer. Although it accounts for only 15% of all lung cancers, its three-year survival rate is just 15%, due to its rapid progression and late diagnosis, which usually excludes surgical options. The current treatment consists of a combination of chemotherapy and immunotherapy, but SCLC is known for its strong ability to develop resistance and metastasize. However, this new study opens a promising pathway for tackling the disease.
"We observed that combining immunotherapy and chemotherapy with a MET inhibitor makes immunotherapy more effective, increasing both survival and tumor response in mouse models," explains Dr. Edurne Arriola, lead author of the study, researcher in the Cancer Molecular Therapy Research Group, Head of the Lung Cancer Section at the Hospital del Mar Medical Oncology Department, and researcher at CIBERONC. This study represents the culmination of more than ten years of research.
A Boost for Immunotherapy
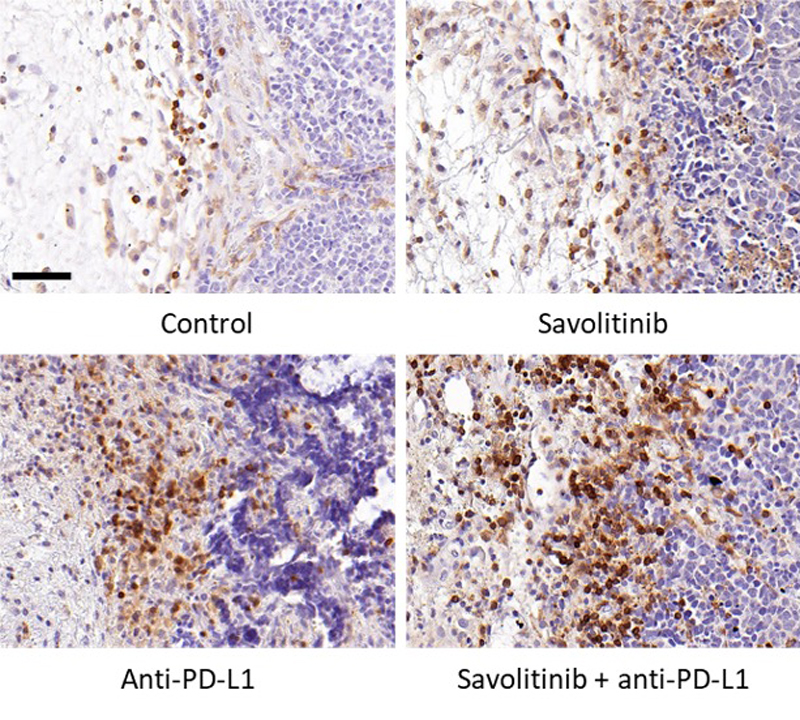
The study analyzed the response to various treatment combinations in mouse models of small cell lung cancer. One group served as the untreated control, another received chemotherapy alone, a third group was treated with chemotherapy and immunotherapy using an anti-PD-L1 monoclonal antibody, and the final group received chemotherapy, immunotherapy, and a MET inhibitor. The best results, in terms of both tumor progression and mouse survival, were observed in the group treated with the MET inhibitor in addition to chemotherapy and immunotherapy. In fact, six out of nine tumors treated with this combination showed a complete response.
Dr. Arriola notes that "this strategy slowed tumor growth and in some cases, completely suppressed it. When we analyzed survival and tumor progression, mice treated with the MET inhibitor had better survival outcomes." This positive and long-lasting response is attributed to the inhibitor's ability to counteract the MET gene's influence on the tumor microenvironment. When MET is inhibited, "the tumor microenvironment-which contributes to treatment resistance-changes, making it easier for immune system T cells, activated by immunotherapy, to act," she adds. In other words, the inhibitor does not act directly on the tumor, but rather facilitates the effectiveness of standard treatment.
The researchers validated their findings using human tumor samples. They observed that in cases where the MET gene is overexpressed, patients have a worse prognosis, with a tumor microenvironment that impairs the effectiveness of immunotherapy and contributes to greater treatment resistance. The same phenomenon was noted with chemotherapy. This is a relevant discovery, as half of the patients with this type of tumor show MET overexpression.
The next step is to initiate a clinical trial in SCLC patients. The goal is to determine whether adding the MET inhibitor after the initial chemotherapy and immunotherapy phase, during maintenance treatment with immunotherapy alone, can prevent tumor progression.
Members of the Research Team
Reference article
Del Rey-Vergara R, Galindo-Campos MA, Rocha P, Carpes M, Martínez C, Masfarré L, Menéndez S, Quimis F, Rossell A, Iñañez A, Pérez-Buira S, Rojo F, Gimeno R, Isla D, Zugazagoitia J, Martí Blanco C, García-Campelo R, Moreno-Vega A, León-Mateos L, Callejo Mellén Á, Park KS, Heeke S, Heymach JV, Taus Á, Paz-Ares L, Rovira A, Arriola E. MET pathway inhibition increases chemo-immunotherapy efficacy in small cell lung cancer. Cell Rep Med. 2025 Jul 15;6(7):102194. doi: 10.1016/j.xcrm.2025.102194. Epub 2025 Jun 20. PMID: 40543507.
Servei de Comunicació:
Marta Calsina Freixas(ELIMINAR)
Tel:
(+34) 93 316 06 80
Doctor Aiguader, 88
08226 Barcelona
© Institut Hospital del Mar
d'Investigacions MèdiquesLegal Notice and Privacy Policy | Cookie Policy | Site Index | Accessibility | Find Us | Contact