
05/10/2022 - Press release
A study led by researchers at the Hospital del Mar Medical Research Institute (IMIM-Hospital del Mar) has determined the role that fibroblasts, the cells that contribute to tissue formation, play in a tumour's ability to generate resistance to the most common biological treatment for HER2.
The paper, published in the journal Nature Communications, demonstrates the ability of a new therapy, currently undergoing clinical trials, to promote a potent immune response by binding to the fibroblasts, enabling it to overcome resistance to anti-HER2 therapy in tumours with this cancer cell protection mechanism. To demonstrate this, the researchers created a 3D tumour model in which they were able to check the relationships between all the factors involved.
HER2+ breast cancer is one of the most aggressive and rapidly progressing cancers. HER2-targeted treatments have changed the outlook, but resistance continues to hinder the curative potential.
Research into cancer treatment resistance is yielding very encouraging results thanks to projects led by researchers from the IMIM-Hospital del Mar cancer research programme.
The microenvironment surrounding tumors in HER2+ breast cancer protects them and helps them develop resistance to the most widely used treatment, the monoclonal antibody trastuzumab. And a particular type of cell in this microenvironment, fibroblasts, plays a key role in this process. These cells have the ability to block the immune system and thereby protect the tumour. Finding a way to overcome this boosts the treatment's capacity to kill tumour cells.
From left to right, Alba Recort, Jordi Badia, Jenniffer Linares, Alexandre Calon, Anna Sallent and Joan Albanell.
Specifically, it is the presence of TGF-beta-activated fibroblasts, which express a molecule called FAP, that protects the tumour from the action of immune cells. Trastuzumab has the ability to target cancer cells that present high levels of the HER2 protein, and when it binds to the cancer, it activates a strong immune response, which is a major contributor to its efficacy against the tumour. However, in many tumours, the immune system is unable to break through the microenvironment surrounding the tumour to eliminate it. This leads to treatment resistance and increases the capacity of this type of cancer to evade the drug and proliferate further. This mechanism was discovered by a team of researchers from the IMIM-Hospital del Mar and the CIBER Cancer Research Centre (CIBERONC) in a study that has been published in the journal Nature Communications.
The authors have also identified a way to overcome the tumour's ability to protect itself and allow the immune system to act on the tumour cells. Using an ex vivo model, i.e., a model that includes living cells from breast cancer patients, the researchers have shown that by targeting the fibroblast-expressed FAP molecules with immunotherapy, this ability to prevent access by immune cells can be reversed. "When this molecule, FAP-IL2v, is added to a tumour recreated ex vivo that contains this treatment-resistant microenvironment, in contact with immune cells, trastuzumab's effectiveness is restored", states Dr. Alexandre Calon, senior author of the research and head of the Translational Research in Tumour Microenvironment Laboratory at the IMIM-Hospital del Mar. It should be noted that the model generated uses human cells and is also applicable to other types of tumours.
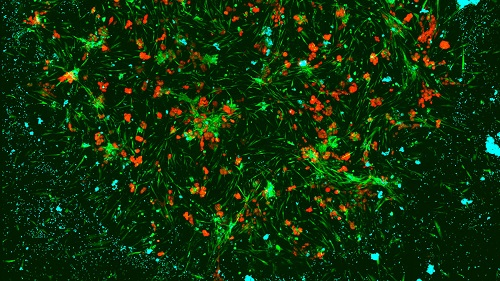
Confocal microscopy of a fully humanized immunocompetent ex vivo model of HER2+ breast cancer recapitulating biological processes that are associated with patient response to treatment.
The study has validated the results with three cohorts of patients and more than 120 samples. In all of them, the levels of fibroblast activation were found to be directly related to the immune system's ability to act on the tumour. The higher the levels, the greater the difficulty in accessing and eliminating tumour cells despite the action of trastuzumab. Dr. Calon emphasised that this facilitates a better selection of patients who will benefit from FAP-IL2v treatment aimed at deactivating the action of the tumour microenvironment. "If we filter people based on these characteristics, we can isolate a population of treatment-resistant patients who can be targeted with this molecule to restore the effectiveness of the breast cancer therapy", he explains.
There are already drugs available that can be used to achieve this effect, although further studies must be carried out to evaluate their application in patients, as Dr. Joan Albanell, head of the Oncology Department at the Hospital del Mar, Director of the Cancer Research Programme at the IMIM-Hospital del Mar and co-author of the study, points out. "The study identifies tumours in which anti-HER2 therapy resistance is caused primarily by one type of fibroblast rather than other causes. This important discovery should be used to design clinical trials with drugs that overcome this resistance only for those patients in whom this resistance is operative. This is where we need to move towards precision oncology", adds Dr Albanell.
The work was carried out in collaboration with researchers from the Barcelona Institute for Research in Biomedicine (IRB) and the Institute for Bioengineering of Catalonia (IBEC), as well as the INCLIVA Health Research Institute in Valencia, and with the support of the Cellex Private Foundation, the Carlos III Health Institute and the Spanish Association Against Cancer.
Cancer immunotherapy at the IMIM
The application of immunotherapy is one of the strategic lines of cancer research being carried out at the IMIM-Hospital del Mar. There are currently several projects underway, with very encouraging results, aimed at validating ways to increase effectiveness or to determine new approaches to facilitate their application.
Reference article
Rivas, E.I., Linares, J., et al. Targeted immunotherapy against distinct cancer-associated fibroblasts overcomes treatment resistance in refractory HER2+ breast tumors. Nat Commun 13, 5310 (2022). https://doi.org/10.1038/s41467-022-32782-3
Servei de Comunicació:
Marta Calsina(ELIMINAR)
Tel:
(+34) 93 316 06 80
Doctor Aiguader, 88
08226 Barcelona
© Institut Hospital del Mar
d'Investigacions MèdiquesLegal Notice and Privacy Policy | Cookie Policy | Site Index | Accessibility | Find Us | Contact